Tens of thousands of grocery store items play up the fact that they are “reduced-fat”, reflecting both the government’s advice about eating less fat, and our concerns about becoming overweight or obese. Our food-shopping habits have changed over the past fifty years, as warnings were posted by the American Heart Association, Department of Agriculture Food Guides, and other agencies that became alarmed at the risk posed by fats, particularly of the ‘saturated” type, for heart disease and other medical problems.
The beginnings of the fat hypothesis
In America, the focus on dietary fat began in the 1950s, through the efforts of the University of Minnesota physiologist Ancel Keys. After the end of the second World War, the incidence of heart disease began to increase, creating fears about an epidemic. In Britain there were similar large increases in the number of deaths from heart disease. Keys went around the world looking for clues to this increase by comparing the diets of different groups of people, and whether these were related to their levels of heart disease. What he saw was that people who consumed more fat had more deaths from heart disease, as shown in this graph from 1952.
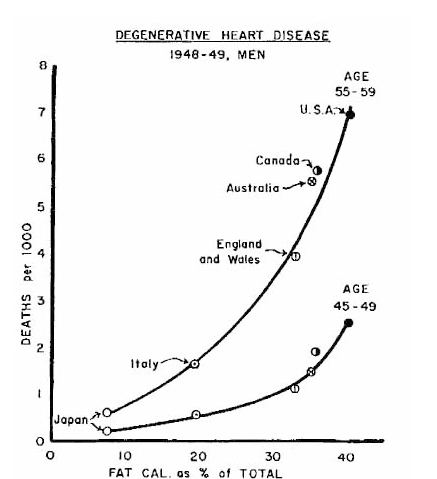
In countries such as Italy and Japan, where people consumed less fat, there were fewer deaths, per capita, than in the USA or Canada, where fat provided more dietary calories. Keys presented his data at a meeting of the World Health Organization in 1952, stating that “. . . fatty diet raised serum cholesterol, atherosclerosis, and myocardial infarction.” (Cholesterol deposition being a characteristic of clogged arteries, atherosclerosis the term for that clogging, and myocardial infarction the medical term for heart attacks.) Despite an initial reluctance to accept his conclusions at face value, over the next decade the medical world gradually came to believe in them. In 1961 a committee of the American Heart Association that included Keys concluded that Americans would reduce their risk of heart disease by reducing the fat in their diets, and by replacing saturated fats with polyunsaturated ones, such as found in oils. Keys, the originator of this hypothesis, was featured on the cover of TIME magazine.
Studies of the fat-heart attack nexus began to accumulate, as did government committees hearing from experts about how to help Americans avoid heart disease. The definitive government response was the report of a special committee headed by Senator George McGovern, which met on and off from 1968 until 1977. This committee initially focused on the origins and effects of hunger and malnutrition in America, and highlighted important concerns in those areas. Legislation followed that amended the existing National School Lunch Act and the Child Nutrition Act. The committee added the topic of “over-nutrition” to its agenda, and when it finished its work in 1977 it issued a document called “Dietary Goals of the United States.” This document changed nutritional policy and solidified the fat hypothesis. It was written by a McGovern staff writer named Nick Mottern, a former labour reporter for The Providence Journal. Mottern had no scientific training, and had not previously written about medicine or science, so he called on an expert to advise him. That advisor was the Harvard nutritionist Mark Hegsted. Two key recommendations of the Mottern report were, to increase carbohydrate consumption to 55-60% of total calories, and to reduce fat consumption to 30% of calories. The work of the committee, culminating in this report, led to the issuing of the Dietary Guidelines for Americans, which have been revised every 5 years since. Fat was now an official enemy of good diet and health.
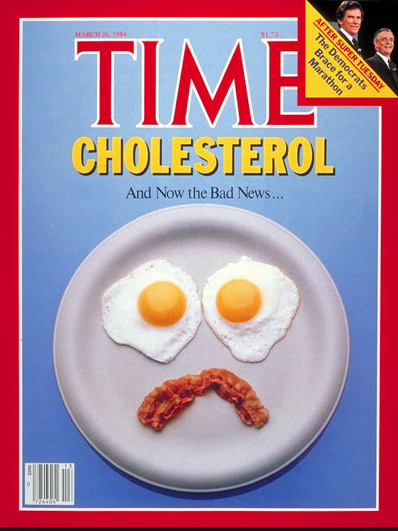
The general attitude toward fat in the diet was captured by a cover on TIME magazine from 1984:
Problems with the fat hypothesis
The fat hypothesis was part of an attempt to understand a perceived epidemic of heart disease after the end of World War II. But what if there was no epidemic? That’s exactly what statisticians at the National Center for Health Statistics concluded. By the end of the War, the availability of antibiotics, and other medical advances, had reduced deaths from infectious diseases, and improvements in living conditions had lengthened lifespans to the point that more and more people were living long enough to have heart attacks. The risk of dying from a heart attack at any particular age remained unchanged (subsequently it has declined as a result of better treatments). Nevertheless, even if there was no epidemic of heart disease, it was still valid to wonder whether diet had something to do with death from it.
It must have seemed self-evident that eating fat, dense as it is with calories compared to carbohydrate or pure protein, would make you fat and would clog your arteries with cholesterol. There was one thing missing from the fat hypothesis, but it was an important piece; there were no strong data supporting it. What had been taken as proof consisted mainly of correlations (you can read about the problem of relying on correlations elsewhere on this website), and unproven assumptions about linkages of events. Even in the early days, a school of thought, championed by the British physiologist John Yudkin, proposed that high sugar consumption was responsible for the high fat levels in the body, not consumption of fat itself. And when better data began to appear, as described below, they didn’t support the fat hypothesis. One of the clearest early criticisms of the fat hypothesis was an article in Science in 2001 by the science writer Gary Taubes. That article is available on-line here. (Taubes has written several books on fat, sugar and diet. His most recent, “The Case Against Sugar” places sugar, instead of fat, in the role of villain in the obesity wars. His writing has won him awards, and is clear, well-informed, and provocative.)
The expert advisor that Nick Mottern relied on to overcome his lack of background in medical science, Mark Hegsted, turned out to be a problematic choice. It has recently come to light that he had previously been the recipient of payments from the Sugar Research Foundation, a lobby group for the sugar industry, to write reviews that downplayed the role of sugared drinks, and focused on fats, as the basis for health problems, including heart disease. These reviews appeared in 1967, in the prestigious New England Journal of Medicine. The issue of Hegsted’s impartiality was brought to public attention in an article in the September 12, 2016 issue of the New York Times. It was based on primary research published in the Journal of the American Medical Association (the abstract can be found here). In crude terms, it appears that a significant part of the support for the fat hypothesis, which led to the Dietary Goals document, was bought and paid for by the sugar industry. Hegsted may have honestly believed what the report concluded, but his contributions were tainted by his previous relationship with that industry. Most scientists would have recused themselves.
(The lobbying continues. In 2015, it came to light that Coke is funding an organization that supports scientists who report that the current obesity epidemic is not due to sugary drinks such as Coca-Cola.)
To make things even more difficult, attempts to corroborate the earlier fat-heart disease relationship have not been successful.
The difficulty of making valid conclusions about human nutrition
Understanding the effects of diet on human health isn’t rocket science, it’s much more complicated than that. As research about the effects of fat continued, it became clear that the important variables were many and included the type of fat, the genetics of the person consuming them, the composition of the rest of the diet, even the age of the subjects of study. We know a lot about human nutrition, including the micronutrients (vitamin and minerals) required for good health, and what they do. We have detailed molecular knowledge about metabolic pathways. We know how much nourishment a person needs, and the effects of age, gender, health, and so forth on those needs. But what we lack, despite the claims of experts such as Dr. Oz, is a solid understanding of the effects of complex diets on human wellbeing, and how to deal with our apparent lust for food and consequent weight gain (caloric consumption per capita has increased by 20% in America between 1970 and 2010).
It’s technically difficult to determine the effects of diet on human health. Studies of large groups of people, measuring variables of their daily lives, including diet and medical events, are of some use, particularly if they are large enough and continue for long enough. The Framingham study, begun by Harvard University researchers in 1948 and continuing today, has provided many clues to the relationship of diet to health. Such studies are expensive, and intrinsically limited. Depending, wholly or in part, on self-reporting (what do you eat for breakfast? how often do you snack? how many ounces of alcohol do you consume each day?) is notoriously unreliable. What to do? The best nutritional studies are “interventional”. Diets are dispensed to randomly assigned control or intervention groups under carefully controlled conditions, and the results are monitored. Understandably, such studies are difficult to do over long periods; people get tired of being told what to eat. Did I mention that they are expensive? They are very expensive; hundreds of millions of dollars have been spent on various kinds of diet-health investigations. Fortunately, all of this effort and expense has produced some results worth knowing about regarding the fat hypothesis, and these will be summarised below.
There’s also the problem of statistics. Most people have a poor understanding of what statistical data tell us (I confess to being less sophisticated than I should be). But there is one aspect that is important to understand in research in which the results are not overwhelmingly clear (fat hypothesis-related studies are in that category). This can be understood by a kind of thought experiment. If the truth is that fat consumption does not cause early death from heart disease, and 100 studies are done to test that hypothesis, most of the studies will show a small effect, either positive or negative. The average result of all studies will probably be zero, or almost zero.That’s the nature of nature. Unless we study an infinite number of people, and control all other variables perfectly, there will always be a significant margin of error in the result. In this case, even if only well-done studies are included, some will come in on the plus side (fat in the diet causes early death from heart disease), some on the negative. Both will have margins of error that overlap the null hypothesis (fat doesn’t cause early death). Statisticians have created a method called “meta-analysis” to reduce this problem, and extract the strongest conclusions from studies. That method combines the outcomes of all good studies on a subject and comes up with the best available answer. What constitutes “good” is itself an issue, but the general idea is clear; improve the strength of the conclusions by including large numbers of studies. Meta-analysis has something to say about the fat hypothesis, as explained below.
So, how’s the fat hypothesis doing?
The results of careful interventional studies began to appear in the 1980s. The outcomes were, as expected, scattered; some found linkages between fat consumption and heart disease, some didn’t. Some studies found a reduced risk of heart disease with increased fat consumption. This is all as expected if there was a small, or no, effect. Rather than chew through the history of these studies, which, trust me, would not be illuminating, I have let professionals do the digesting, so to speak, by meta-analysis.
One of the most respected entities for resolving complex questions about human health is The Cochrane Collaboration. Cochrane is a huge, non-governmental, international, network of scientists and physicians who periodically undertake large-scale analyses of medical questions. In 2001, this organisation summarised studies of the effects of reduced or modified fat consumption on the incidence of cardiovascular disease, or mortality from heart disease or all causes. This review was updated and enlarged in 2011, when it included subjects from 48 interventional studies (1). Finally there was some solid evidence for the effects of fats on heart health; but the conclusion was not exactly what the fat hypothesis predicted. Replacing saturated fat with unsaturated fats, when done in the context of a more comprehensive dietary plan, or care intervention, did reduce the risk of heart disease somewhat (for men, but not women). However, replacing the calories derived from saturated fat with protein or carbohydrate (i.e., a low-fat diet) did not. Finally, modifying fat intake (either reducing fat, or replacing saturated fats with unsaturated fats or protein) had no effect on mortality, either from heart disease or from all causes.
PLAIN LANGUAGE SUMMARY OF THE 2011 COCHRANE REPORT (Partial)
Cutting down or changing the fat we eat may reduce our risk of heart disease.
Modifying fat in our food (replacing some saturated (animal) fats with plant oils and unsaturated spreads) may reduce risk of heart and vascular disease, but it is not clear whether monounsaturated or polyunsaturated fats are more beneficial. There are no clear health benefits of replacing saturated fats with starchy foods (reducing the total amount of fat we eat). . . Modifying the fat we eat seems to protect us better if we adhere in doing so for at least two years.
The lack of effect of a low-fat diet for reducing coronary heart disease for women was also found in the large “Women’s Health Initiative” study in 2008 (2).
Earlier, Cochrane had looked at a larger pool, almost a million people, to see whether education programs to modify a broad group of risk factors for heart disease, “Healthy Heart Programmes”, had an effect on morbidity or mortality due to coronary heart disease (the study can be found here). These risk factors included high cholesterol, excessive salt intake, high blood pressure, excess weight, a high-fat diet, smoking, diabetes, and a sedentary lifestyle. Sadly, these education programs did not reduce either the risk of heart disease or death.
Another analysis of randomized, controlled dietary trials in 2016 concluded: “The current available evidence found no significant difference in all-cause mortality or CHD [coronary heart disease] mortality, resulting from the dietary fat interventions.” It further concluded that the “. . . evidence currently available does not support the current dietary fat guidelines.” (3) The conclusion about the lack of effect of fat intake on mortality is in agreement with the Cochrane report in 2011.
What are these authors referring to as “current dietary fat guidelines”? Well, as of January, 2016, the US Department of Agriculture’s “Healthy Eating Style” recommends: “. . . replace sour cream, cream and regular cheese with low-fat yogurt, milk and cheese” and “Choose fat-free milk, yogurt, and soy beverages (soy milk) to cut back on saturated fat.” and further “Choose vegetable oils instead of butter, and oil-based sauces and dips instead of ones with butter, cream, or cheese.” The third recommendation, although not the first two, is supported by the 2011 Cochrane report, which found a small reduction in heart attack incidence, although not deaths, for modified fat diets (unsaturated fats in place of saturated). Fat reduction, though, didn’t make a difference.
There is another hypothesis out there that increasing numbers of nutritional scientists are paying attention to. That one also began a long time ago, and came out of Britain; that would be Yudkin’s idea, already mentioned, that the real dietary culprit accounting for our growing obesity and heart disease is sugar. But that’s another story.
As for the fat hypothesis: it appears to be a zombie that cannot be killed. Probably because it has a slight connection to something real (good to replace saturated fat with unsaturated), although it’s not the original hypothesis that fat causes death.
Go to Latest Posts
- Hooper, L., C. D. Summerbell, R. Thompson, D. Sills, F. G. Roberts, H. Moore, and G. Davey Smith. 2011. Reduced or modified dietary fat for preventing cardiovascular disease. The Cochrane database of systematic reviews:Cd002137.
- van Horn, L., and J. E. Manson. 2008. The Women’s Health Initiative: Implications for clinicians. Cleveland Clinic Journal of Medicine 75:385-390.
- Harcombe, Z., J. S. Baker, J. J. DiNicolantonio, F. Grace, and B. Davies. 2016. Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis. Open heart 3:e000409.