Human energy metabolism, the science behind the energy provided by the food we eat, is a complicated subject. I taught it to science and medical students for more than 35 years, but its intricacies continue to surprise and entertain me. I don’t provide nutritional advice, but I want to blow away some of the cobwebs surrounding it. Much of the material summarized here is described in more detail in previous posts, which are linked.
Why calorie counting has a bad name
The aphorism ‘calories in equal calories out’, or CICO, is seen differently by scientists and most diet commentators. We scientists believe that the laws of thermodynamics are as true for human nutrition as they are for all chemical and physical reactions. But many nutritional commentators or advisors argue that this is not so: CI may not equal CO, depending on what kind of food we eat, and what else is in our system.
Scientists are right, thermodynamics does apply, but it’s also true that CICO is a little simplistic. What people who argue that CI isn’t necessarily equal to CO are often referring to is the fact that consumption of a nominal number of food calories doesn’t always lead to a predictable effect on body weight. Often, those calories behaved like there were more, or fewer, of them than listed.
One reason that diet experts sometimes tell you that CICO doesn’t explain things is that it takes energy to digest food, and it takes different amounts of energy to digest protein, carbohydrate, and fat. So, if you base your calculations on the usual numbers (4 Cal/gram protein, etc.) you’ll get it wrong. But the original assignment of 4 Cal/gram protein actually took digestion into account: the bomb calorimeter said protein gives off 5.6 Cal/gram of energy on combustion, but the people doing the work were smart enough to figure out that about 1.6 Calories were required for digestion, so the 4 Calorie number is probably right. Nice try.
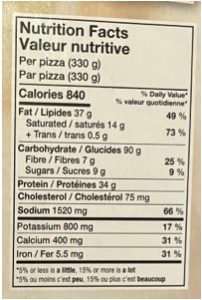
You might think that looking up your own calorie requirement, and then reading the information about the foods you consume, would allow you to tailor your intake to your needs exactly. Whether it’s to lose weight, stay the same, or gain weight. You’d be wrong. The calories listed for many foods, particularly highly processed ones, are often wrong. Researchers in Australia found that packaged food contained anywhere between 13% less and 61% more calories than the packaging stated (1)
Particularly unfortunate is that ‘low calorie’ items in restaurants were the ones most likely to understate their calorie content. And it would often be just that kind of dish you would order if you were watching your weight. For example, a classic blue cheese wedge side salad at a particular steak house in the US, described as containing 376 Calories, had a whopping 1,035 (1). This very problem has been noted by frustrated dieters – they counted the calories listed, and gained, or didn’t lose, weight.
Junk food
A recent post (here) examined a study that looked at the effects of a highly processed, aka junk, food diet. That study, which was well structured and carefully done, showed that junk food induces us to eat more than we need, and that the extra calories then go to the laying down of fat. The popular diet advice literature abounds with explanations for the effects of junk food, many of which involve hormone responses and other sophisticated explanations. While these may be relevant, the effect of junk food is more basic: it induces excess consumption. And the result is weight gain.
The Reasons for ‘Slow Metabolism’
Interest in the CICO issue is often related to a person’s perceptions that i) calorie counting isn’t helping me to lose weight, and ii) others seem to be able to eat as much or even more than me, but I’m gaining weight, and they aren’t. The latter conundrum is sometimes referred to as “I have slow/low metabolism”, or “My friend is so lucky. She has fast metabolism.”
The reason calorie counting often doesn’t work is partly explained previously. The business of slow and fast metabolism, however, is something else entirely. In fact, some people do have ‘faster metabolism’ than others.
One factor that can affect energy metabolism is the ‘fidget factor’; some people move around more than others, and that muscle activity uses calories. (Think leg-jiggle.) As a result, they burn more calories in basic, day-to-day activities.
A more important factor is Basal Metabolic Rate (BMR). (You may have heard about Resting Metabolic Rate, or Resting Energy Expenditure. For this discussion, those are essentially the same as BMR.) BMR is the energy we consume at rest. It is measured after a few hours of sleep, at peace with the world (psychic state matters).
BMR is the energy that the body needs to stay alive (I have a post about that here). The liver, the lungs, the heart, and particularly the brain, which consumes about 20% of the energy burned at rest. Quite a lot of the resting energy expenditure goes to getting sodium out of cells and potassium in. BMR makes up about 60-75% of the daily energy requirement for most people (obviously not for a rider in the Tour de France). All of this happens continually, whether we’re awake or sleeping, whether we’re lounging in front of the TV or running a marathon.
BMR is correlated with a body’s ‘fat free mass’, in other words, it’s proportional to the weight of the body that isn’t fat. (Fat consumes relatively little energy.) And that proportionality holds whether you’re male or female, young adult or old. (The very young are different – they need more energy relative to their fat-free mass because they’re growing and have a high surface-to-volume ratio, and lose heat fast.) Females and old people generally have less fat-free mass (less muscle, basically), and thus have lower BMRs.
Here’s where it gets a little messy. If you plot a large number of people’s BMR against their fat-free mass, you do get a trend, but you also get scatter (as discussed in the previous post). Two adults with the same fat-free mass may have a 30% difference in their BMR, and this give them ‘faster’, or ‘slower’, metabolism.
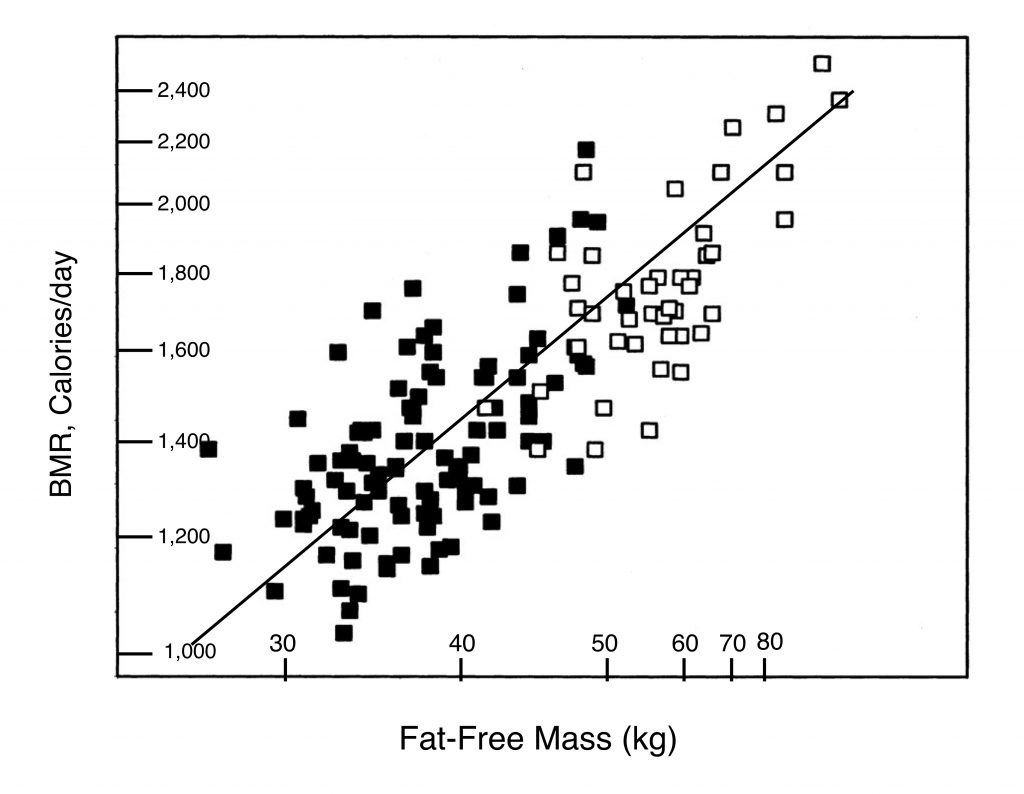
There are complicated metabolic reasons, mostly resulting from genetics, that help explain the scatter in the BMR vs fat-free mass graph. In general terms, they boil down to people having more or less ‘efficient’ energy metabolism. One person has a BMR of X calories, while another, 120% of X. The ‘extra energy’ goes to heat, which the body is quite good at dissipating. (Around 50% of the energy we consume goes to heat anyway; some people generate even more.) The variation in BMR is responsible for at least part of the frustration felt by people who gain weight when they eat the same amount as a friend who doesn’t.
Since people with the same build and weight may have different BMRs, it would be impossible to prescribe a ‘weight-loss’ diet knowing only their fat-free mass and the desired end-point for the diet. A difference of 15% in BMR between two people like that could mean a weight difference of 35 pounds in a year.
BMR is largely genetic, but not entirely (2). Since it’s related to fat-free mass, increasing muscle mass will increase BMR (and losing muscle through age or illness will decrease it). Exercise therefore can lead to weight loss for two reasons – because of the energy spent exercising, and because it leads to an increased BMR. But again, diet is of greater importance – eating more after exercising can negate any advantage of exercise with respect to body mass.
One of the most intriguing forms of exercise is High Intensity Interval Training, which I have reviewed in detail elsewhere. Some diet commentators have noted that HIIT can increase BMR for as long as 48 hours due to post-exercise effects, but overall, HIIT doesn’t change BMR (3).
The value of Body Mass Index (BMI)
Body Mass Index, defined as body weight in kilograms divided by the square of height in meters, has been used for about 200 years to assign underweight, overweight, normal or obese labels to bodies. But applied to a single person, of and by itself, it isn’t necessarily a good estimator of body health — Arnold Schwarzenegger in his bodybuilding prime (as shown at the top of this post) had a BMI of about 31, which is considered to be ‘obese’. His high BMI was, of course, due to Mr. Universe’s massive musculature, which made him look, in the unkind words of the essayist Clive James, like a condom filled with walnuts.
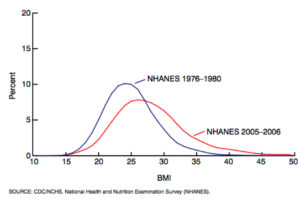
BMI is a useful monitor of a person’s progress in weight control, but that can be determined by simply stepping on the bathroom scale. Where it is very useful is as a measure of the health of a group, or of the population as a whole. And there, it has a sobering message for us. As described elsewhere, our North American BMI has gone up, a lot, over the past 50 years. And this is because we eat a lot more than we used to, and exercise somewhat less (it seems). There’s a ballooning level of overweight and obese people. So, while having limited value in monitoring personal body health, BMI does fairly accurately reflect population health.
An extreme example of the usefulness of BMI in evaluating a group’s health is found in the Pima Indians of southwest Arizona (described here). At the beginning of the twentieth century, the Arizona Pimas were successful farmers in a low-water environment, thanks to their expertise in water management. And they were lean and fit. Today, having been deprived of their source of water, they have largely left farming, and are recipients of large amounts of government ‘aid’ in the form of high-carbohydrate surplus food. And they have some of the highest levels of obesity (70% of adults) and Type 2 diabetes (T2DM) (50% prevalence) in the world (4).
The genetically-related Pima living in the state of Sonora in Mexico are still hard-working farmers. And they have a level of T2DM of 5% and a level of obesity of about 10%, the same as the non-Pimas living near them. Whereas the Arizona Pimas engage in physical activity about 8 hours per week, the Mexican ones do on average 27 hours. The Mexican Pima are still lean and fit, despite taking in about the same number of calories as their Arizona cousins. Calories being burned by manual labor in Mexico are stored as un-needed fat in Arizona.
While BMI is not an absolute measure of health, it does have a significant relationship with staying alive, which is quite an important health parameter. There’s an increased probability of death from all causes as BMI rises into the ‘overweight’ (BMI > 25) range. But the risk doesn’t rise appreciably until BMI is over 30. (There’s also a danger of death for very low BMI). This general trend is true for all age groups (and men and women are similar).
The trends are very similar in Europe, North America, Australia and New Zealand, East Asia, and South Asia. Of course, the overall risk of dying is much higher at age 80 than at 40 (in Canada, about 40 times higher). So the average 40-year-old person with a high BMI will outlive an average fit 80-year-old.
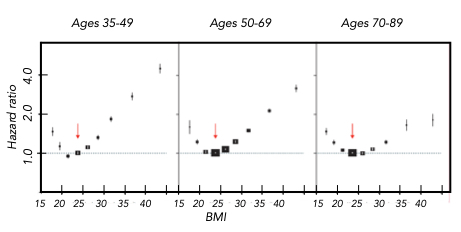
It’s quite noticeable that having a higher BMI is less of a danger at older ages. What you don’t want to be is young and overweight.
What about Atkins? What about Ozempic?
There are certainly diets and drugs that can, at least for some people and for a time, lead to weight loss. (In fact, almost any diet can do this for a while by the placebo effect.) What about the famous Atkins diet, in which the consumption of carbohydrate is severely restricted? The body needs quite a bit of carbohydrate to function normally (during long-term starvation it adapts to a lower carbohydrate requirement). But because the brain depends on glucose, as do the red blood cells, the average adult body needs to consume about 200 grams of glucose a day. But the Atkins diet, even during the maintenance phase, typically provides only 50-100 grams of carbohydrate a day (that includes starches, which can be converted to glucose).
The body is well equipped to handle such a carbohydrate deficiency: there’s a pathway for converting amino acids, derived from dietary protein or from the body’s own protein, into glucose. It’s called gluconeogenesis (synthesis of new glucose). Not surprisingly, there’s also an energy price for this pathway. And this leads to a higher energy consumption overall (6). Even with no increase in exercise, there will be a relative caloric deficiency in the Atkins diet, that is, an increase in BMR.
As well as spontaneously increasing the Basal Metabolic Rate, a low carbohydrate diet suppresses appetite (7, 8). There’s an increase in BMR, due to the energy cost of gluconeogenesis, and a decrease in food intake due to appetite suppression. Win-win for the Atkins dieter. However, a low-carbohydrate diet can also reduce the interest in exercise, which is not useful for weight loss.
There’s a current surge of interest in a class of drugs (‘GLP-1 agonists’) that includes the drugs Ozempic, Wegovy, and others. The GLP-1 agonists affect metabolism in various ways, including effects on the hormones insulin and glucagon, but the most important weight-loss effect is that they reduce appetite (9). (However, they somewhat increase the risk of pancreatitis, gastroparesis, and bowel obstruction (10)).
What worked for my friend
As we scientists say, a single case is an anecdote, not science. Nevertheless, I think the experience of a friend, a guy I have known forever, is intriguing. Perhaps partly as a result of the stresses of life, he found himself gaining weight in late middle age. An active gym goer in his earlier years, he had begun to lose interest in working out, and to gain interest in ‘reward’ eating (and drinking), with the result that he graduated from the ‘normal’ BMI range all the way to ‘obese’ in a decade. At that point, he decided to do something.
‘Something’ involved two complementary changes: going to the gym several times a week, and being more aware of his diet. He didn’t yet know about the new-age term ‘mindful eating’. The newsletter of the T. H. Chan School of Public Health at Harvard University says that “Mindfulness is an intentional focus on one’s thoughts, emotions, and physical sensations in the present moment.” A review of a book on ‘mindful eating’ (Vancouver Province, February 20, 2012) stated that mindful eating “. . . incorporates more of a Zen approach rooted in Buddhist teaching by raising your level of consciousness of why and how you eat, internal and external responses and physical sensations to food.”
My friend wasn’t a new-ager, and wasn’t up on the mindful eating literature, which has blossomed recently. But thinking about eating, and being sensitive to its effects, made some sense. It suggested to him that it would be a good idea not to eat if he wasn’t hungry. Even skipping, or skimping on, a meal from time to time.
When he started at the gym, my man was thinking that a workout would burn up some calories, which it does. However, the few hundred calories consumed was only part of the benefit. Unknown to him until years later, the buildup of muscle as a result of lifting heavy things and pumping peddles also increases the Basal Metabolic Rate. A study which is a meta-analysis of many others presents the evidence that a combination of diet and exercise is a more effective weight loss program than diet or exercise alone (11).
One of the biggest hurdles to losing weight is eating late in the day. So my friend began to eat his biggest meal at lunchtime. And when the munchies struck after 6 PM, as they sometimes do, he would ask himself, “Am I really hungry? If I only desire chocolate or booze, not cheese on toast, I’m not really hungry.”
He gave up most highly processed foods. He had read somewhere that stepping on the bathroom scale every day was a good idea, so he did that most mornings.
Although the first pounds came off quickly, further change was slow. But it was rewarding. Over 18 years he has lost about 50 pounds, and the weight is staying off with almost no effort.
Is my friend just genetically lucky, as someone who can easily carry out and benefit from this simple, sensible, program of weight loss? Who knows. But in his new-found state, he is now unconsciously depending on what the American physiologist Walter Cannon wrote a book about in 1932: Cannon called it ‘The Wisdom of the Body’. Part of that homeostatic mechanism is the innate ability of our bodies to regulate food intake. A new incarnation of the ‘mindful eating’ paradigm is ‘listen to your body’.
How is it that our bodies are so exquisitely tuned to avoid overeating?
I hate to say this, but it’s complicated. Many physiological factors contribute to keeping the balance, and we are still learning about them. There is cross-talk between the hypothalamus, the gastrointestinal tract, and our adipose tissue. Leptin, the ‘satiety hormone’, and ghrelein, the ‘hunger hormone’, deliver signals to various organs. We’ll never equal the wonderful harmony of the well-tuned body by taking drugs.
Go to Latest Posts
References
- Restaurants’ Calorie Counts Are Wrong, Research Finds. Williams, Sarah C. P. Live Science, published July 19, 2011. https://www.livescience.com/15123-restaurants-calorie-counts-wrong-research-finds.html
- Genetic and environmental factors in relative body weight and human adiposity. Maes, H. H., M. C. Neale, and L. J. Eaves. Behavior genetics 27:325-351 (1997).
- Impact of 4 weeks of interval training on resting metabolic rate, fitness, and health-related outcomes. Schubert, M. M., H E. Matthew, H. E. Clarke, R. F. Seay, and K. K. Spain. Appl. Physiol. Nutr. Metab. 42(10):1073-1081 (2017).
- Diabetes mellitus in American (Pima) Indians. Bennett, P. H., T. A. Burch, and M. Miller. The Lancet 298:125-128 (1971).
- Body-mass index and all-cause mortality: individual participant data meta-analysis of 239 prospective studies in four continents. The Global BMI Mortality Collaboration. The Lancet 388:776-786 (August 20, 2016).
- Gluconeogenesis and energy expenditure after a high-protein, carbohydrate-free diet. Veldhorst, M. A. B., M. S. Westerterp-Plantenga, and K. R. Westerterp. Am. J. Clin. Nutr. 90:519–26 (2009).
- The effects of a low-carbohydrate ketogenic diet and a low-fat diet on mood, hunger, and other self-reported symptoms. McClernon, F. J., W. S. Yancy Jr., J. A. Eberstein, R. C. Atkins, and E. C. Westman. Obesity15(1):182-7 (Jan. 2007).
- Perceived hunger is lower and weight loss is greater in overweight premenopausal women consuming a low-carbohydrate/high-protein vs high-carbohydrate/low-fat diet. Nickols-Richardson, S. J., M. D. Coleman, J. J. Volpe, and K. W. Hosig. J. Am. Diet. Assoc. 105(9):1433-7 (Sept. 2005).
- Effects of GLP-1 on appetite and weight. Shah, M., and A. Vella. Rev. Endocr. Metab. Disord. 15(3):181-7 (Sept. 2014).
- Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. Sodhi, M., R. Rezaeianzadeh, A. Kezouh, et. al., J. Amer. Med. Assoc. 330(18):1795-1797 (2023)
- Impact of long-term lifestyle programmes on weight loss and cardiovascular risk factors in overweight/obsese participants: A systematic review and network meta-analysis. Schwingshackl, L., S. Dias, and G. Hoffmann. Systematic Reviews 3(130). https://www.mcmasteroptimalaging.org/full-article/b0af48fa6a1e736d1dc49f02ddf4003