Sometimes I run into new information about a story I’ve previously posted that has changed my mind. This post is an example. I previously wrote about three cancer myths that I concluded were wrong, including that vitamin C is a potentially useful anti-cancer agent. I’ve now read some work that has changed my mind: I think that vitamin C may have anti-cancer activity, and certainly that it should be investigated further. So this post is a changed version of the earlier one, which appeared in June, 2019. The other two myths still remain counterfactual, at least to the best of my knowledge. They are, that we are in an epidemic of cancer, and that an abortion increases a woman’s risk of later breast cancer. In other words, I still think those two ideas are wrong.
Story #1: The “cancer epidemic” is not what most people think it is.
The linkage between the words “epidemic” and “cancer” is easy to find in stories on the news media, the Internet, and articles on the radio or TV. Those stories usually refer to large increases in the incidence of cancer, and predict even larger ones to come. What is implied is that we are seeing an increased risk of having cancer, and of dying from it. The message that total cancer incidence is increasing is correct, but the implied one about an increasing risk of getting cancer, and dying from it, is not.
The reported incidence of cancer is a result of several factors. Firstly, it is related to age; older people get more cancer than younger ones. As the population ages in the developed world, so the incidence of cancer is also increasing. To make comparisons meaningful, it is standard practice to report both incidence and death rates as “age adjusted” to reflect the changes over time of the real risk. Data are adjusted to reflect a particular age distribution in the population, which in the case of the United States is the age distribution of the 2000 population. This adjustment is applied to data from both pre-2000 and post-2000 distributions.
The apparent incidence will also increase if diagnosis becomes more sensitive — there are more people diagnosed with cancer if it is detected earlier than later in the course of the disease. During the 1980s, new diagnostic procedures allowed doctors to detect breast and prostate cancer earlier. This led to a significant increase in their apparent incidence, as shown in the graph of the incidence of selected cancers in the USA (Figure 1). Naturally, this caused concern, but the new diagnostic methods were detecting both disease and conditions that would not endanger the life of the patient.
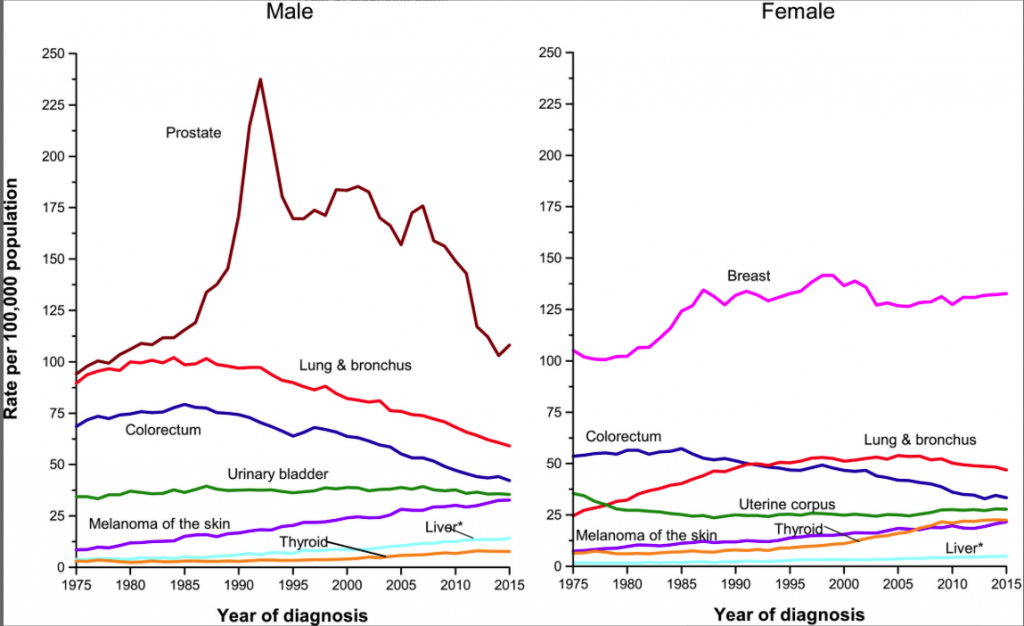
An important aspect of cancer incidence is shown by the curves for cancers of the lung and bronchus. Their incidence reflects the increases, and subsequent decreases, of smoking, which is responsible for most of them. The percentage of men who smoked in the USA peaked around 1960, and the incidence of lung cancers around 25 years later. Women smokers peaked around 1975, and their lung cancer numbers peaked after 2000 and is now slowly decreasing.
While the age-adjusted incidence rates are declining for some cancers (colorectal, prostate), others are increasing. The overall rate of incidence for men and women is decreasing since 1990 (data not shown), and is higher, overall, for men than for women.
Incidence is not an accurate reflection of most people’s greatest fear from cancer: we are usually more concerned about the risk of dying at a given age. This is a “hard” number, not subject to changes in diagnosis. What it shows (Figure 2) for the United States (where statistics are easily available; the developing world presents a different picture), is that age-adjusted death rates are declining. Most of this decline is due to a decrease in lung cancer as smoking rates go down, but some other major cancers (colorectal, prostate, breast) are also showing a steady decrease in the past decades. Better treatment capabilities and diagnostic procedures are in part responsible, but so is a growing awareness of some major risk factors.
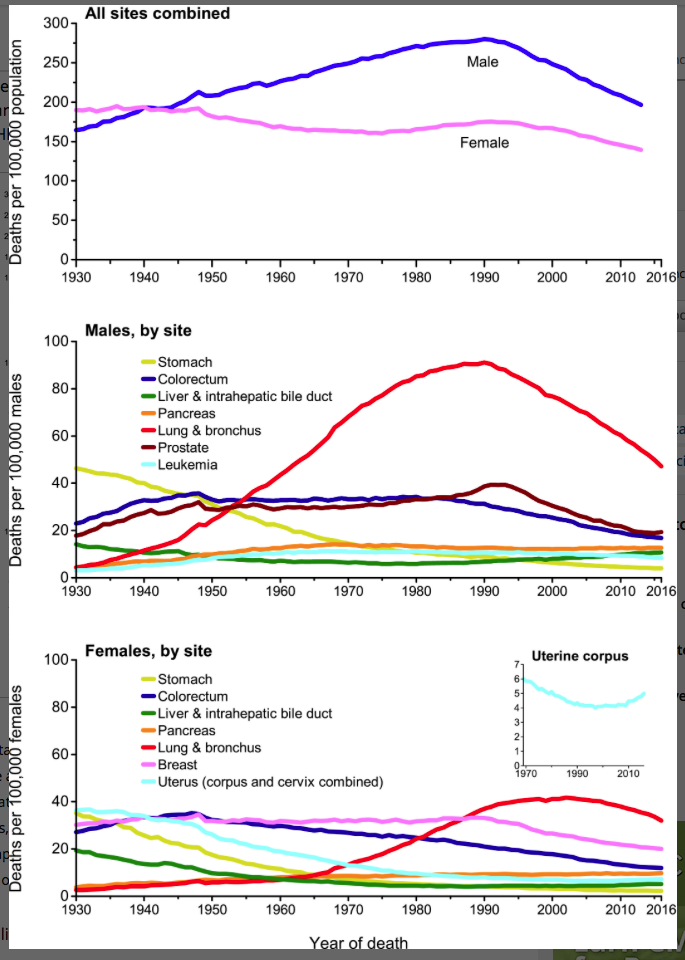
In summary, the total incidence of cancer is increasing as a result of an aging population and better diagnostics. But the risk of dying is, since 1990, on the way down. Once most of the effects of prior smoking pass through, the age-adjusted rates of incidence and death will both be significantly lower.
The origin of story #2: A disturbing report of a link between abortion and breast cancer
In 1981, a publication in the British Journal of Cancer concluded that a first-trimester abortion, whether spontaneous or induced, was associated with a 2.4-fold increase in breast cancer risk in later years (6). The data involved 163 breast-cancer patients, and “support[ed] the hypothesis that an induced abortion can adversely influence a woman’s subsequent risk of breast cancer”, to quote the authors. But they admitted that their data showed inconsistencies, which weakened their conclusions, and that the issue should be re-evaluated with a larger study. In other words, there might be a linkage, but you couldn’t make a statistically strong conclusion based on the available data.
An accompanying editorial, written by an expert on the epidemiology of breast cancer, cautioned that a linkage had not been well established, and also pointed out that women who report induced abortions generally have other unfavorable risk factors in their lives that make interpretation difficult. Although some of these factors had been taken into account in the original report, there were likely to be others that hadn’t. For example, bearing one or more children to term is correlated with a decreased risk of breast cancer. If a woman has had an abortion because she did not want to have children, and never had a child subsequently, she would be in the slightly higher risk group of women who never completed a pregnancy. But the higher risk would have been due to her never having had children, not directly to her abortion.
Not surprisingly, this paper caught the attention of the anti-abortion community. If an induced abortion causes breast cancer, that could be a powerful motivator to not have one. A number of anti-abortion proponents took to saying that this study constituted scientific proof of the linkage, despite the caution expressed by the authors and the editors of the British Journal of Cancer.
Problems with the early study
There are important concerns with studies such as the one that reported an abortion-breast cancer link in 1981. It is an example of a “retrospective” study, in which subjects are asked to recall what they did in the past. Abortion is a sensitive issue for women, and is generally underreported. As such, it is subject to recall bias, which in the case of breast cancer and abortion works like this: if women with breast cancer are more likely to (correctly) tell a researcher that they have had an induced abortion earlier in their lives than women who are healthy, then there will appear to be more abortions in the cancer patient group than in the controls.
Abortion opponents dismiss this possible weakness by saying ‘…Forget an abortion? Not likely!’ But it’s not a matter of forgetting, it’s that healthy women are more likely to keep a past abortion to themselves, whereas women with breast cancer are more likely to disclose such details, perhaps in hopes of aiding research on their disease or even their own treatment. That’s what a 1991 study from the Karolinska Institute in Sweden, a country where all abortions are kept in national records, indicates: women with breast cancer report their history of abortions more truthfully than do healthy women (7). The authors of the Swedish study offered the opinion that this might explain the apparent linkage between abortion and an increased risk of breast cancer found in some, but certainly not all, studies.
The early report of an abortion-breast cancer link involved only 163 subjects. The statistics of that study were considered to be inadequate by commentators, and the authors themselves. Further work by the same researchers, some 15 years later, using a larger data set, failed to show a linkage and thus overturned their earlier, tentative conclusion (8).
No linkage has been established between breast cancer and abortion
The case for an abortion-breast cancer linkage was more or less erased by a paper from the Harvard School of Public Health in 1995 that summarized the findings from a broad, international study (almost 4,000 breast cancer cases). The authors stated ‘These results do not support a large overall association between abortion and breast cancer risk’ (9).
Another wide-ranging study looking at over 3,000 cases and almost 5,000 controls reached the conclusion that ‘the risk of breast cancer is not materially affected by abortion, regardless of whether it occurs before or after the first term‘ (10). More recent support for this conclusion exists in abundance (for example, in (11)).
Perhaps the clearest statement about the lack of an abortion-breast cancer link is contained in a statement of the American Cancer Society (ACS):
“In 2003, the US National Cancer Institute (NCI) held a workshop of more than 100 of the world’s leading experts who study pregnancy and breast cancer risk. The experts reviewed human and animal studies that looked at the link between pregnancy and breast cancer risk, including studies of induced and spontaneous abortions. Some of their findings were:
- Breast cancer risk is increased for a short time after a full term pregnancy (that is, a pregnancy that results in the birth of a living child).
- Induced abortion is not linked to an increase in breast cancer risk.
- Spontaneous abortion is not linked to an increase in breast cancer risk.
“The level of scientific evidence for these findings was considered to be “well established” (the highest level). The American College of Obstetricians and Gynecologists (ACOG) Committee on Gynecologic Practice also reviewed the available evidence in 2003 and again in 2009. In 2009, the Committee said, ‘Early studies of the relationship between prior induced abortion and breast cancer risk were methodologically flawed. More rigorous recent studies demonstrate no causal relationship between induced abortion and a subsequent increase in breast cancer risk.'”
This Cancer Society statement analyzes why some studies are more definitive than others, and summarizes a wide range of international studies which support its conclusion that abortion and breast cancer are not linked.
So, while some people still claim that a linkage exists (see for example here), the evidence is against them. (The proponents of such views are almost always from the anti-abortion, “pro-life”, movement.) The studies that they claim support their case are of the type whose reliability is carefully criticised, and found wanting, in the ACS statement. There is nothing to suggest that the ACS summary, stating that there is no established link, is wrong.
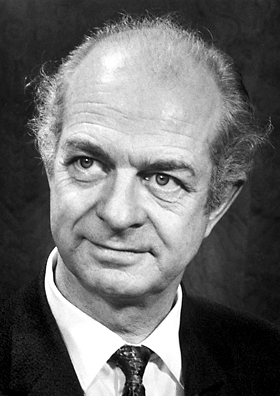
Introduction to Story #3: Linus Pauling was one of the greatest scientists who ever lived
If you ask the average person to name a famous scientist, most people might say “Einstein”. If you press for another name, as likely as not it would be “Pauling”. Linus Pauling made some of the most important contributions to our understanding of the natural world of any scientist of the 20thcentury.
Pauling was born in 1901. He didn’t receive a high school diploma on leaving school (he was too impatient to complete some necessary credits). But he was accepted to Oregon Agricultural College (now Oregon State University) and graduated with a degree in chemical engineering. He was then accepted at one of the most prestigious universities in the world, Caltech, for graduate work. At age 24, he graduated with a Ph. D. in chemistry.
While still in his 20s, Pauling began to study the nature of chemical bonds, and devised a quantum mechanical description of this most fundamental feature of molecular structure. He summarised this work in a book “The Nature of the Chemical Bond” before he turned 40, and won the Nobel Prize in Chemistry for that work in his early 50s. No less a figure than James Watson, co-discoverer of the DNA double helix, has said that this was “chemistry’s most influential book of this century and its effective bible”.
Other profound scientific contributions followed, among them a description of a fundamental structural motif that makes up large parts of protein structures, which Pauling named ‘the alpha helix’. He combined experimental structural work with molecular modeling and a deep understanding of molecular interactions to devise the alpha helix. It is a fundamental part of the vocabulary of protein architecture.
In the field of human genetics, Pauling provided the first explanation for a genetic disease, sickle cell anemia. He headed a study that showed that the change of a single amino acid in the protein chain of hemoglobin, the oxygen carrying molecule in the blood, led to the observed problems for people with two copies of the sickle-cell version of the mutated gene.
And if Watson and Crick had not discovered the double helix, it was Watson’s opinion that Pauling would soon do so. They could feel him breathing down their necks.
Pauling also contributed to a betterment of the human condition
Pauling always maintained a strong anti-war stance, which showed itself in many of his political positions. After World War II, testing of nuclear weapons in the atmosphere became widespread. These tests released a radioactive isotope of strontium, which displaces calcium in the bones and teeth, particularly of young children, and poses a mutational hazard. Like Einstein, Pauling used his prominent stature to promote a public policy; he become a leader of opposition to atmospheric testing by hundreds of prominent scientists and others. He helped gather powerful public and scientific opinion to stop it.
In 1963, President Kennedy of the United States and Premier Nikita Khrushchev of the Soviet Union signed a treaty banning it. The following day, the Nobel Prize Committee awarded Pauling the Peace Prize for his work on getting the ban. Again, as for the Chemistry award, he was a sole recipient, the only person ever to have won two solo Nobel Prizes (Marie Curie won two Nobel Prizes, but shared in the first one, in Physics, with her husband).
Was Linus Pauling right after all?
In Linus Pauling, we have one of the greatest minds in scientific history. We also have another example of an exalted scientist who wandered into an area he knew little about. Based mainly on personal experience, Pauling became convinced that taking large doses of vitamin C was an antidote for the common cold. His 1970 book ‘Vitamin C and the Common Cold’ was a bestseller. This conclusion, however, is not supported by recent studies. He also proposed that it would help overcome a variety of psychiatric conditions, including schizophrenia. This, too, is not supported by data (3).
Pauling then collaborated with a British cancer surgeon, who claimed to find that high levels of Vitamin C would extend the life of terminally ill cancer victims. But other medical scientists subsequently concluded that there is no beneficial effect of Vitamin C, or other vitamins, in cancer therapy (4, 5). Was Pauling wrong? I thought so, based on work from the mainstream of science. I think my conclusion was premature.
The studies of Ewan Cameron (the British cancer surgeon with whom Pauling collaborated) were different from those of the cancer researchers who later claimed his conclusions were not correct. It’s true that the Cameron-Pauling studies were not to the highest standards of today’s clinical investigations. But they were pretty good, and they had one feature that the subsequent dismissive studies lacked: Cameron’s patients received intravenous injections of high levels of vitamin C, while the later investigations provided only oral vitamin C. It is now known that the i.v. protocol results in as much as a 25-fold higher level of circulating vitamin C levels.
More recent work supports the idea that vitamin C may have a useful effect on cancer. These studies are complex in nature, but the bottom line is, that vitamin C, with or without conventional cancer drugs, preferentially kills human cancer cells grown in mice. These are cells carrying mutations in cancer-causing genes (‘oncogenes’) that are found in certain human cancers, such as colon and lung cancers. That work has uncovered a sound metabolic mechanism for why that should be so, which is itself an exciting new development. That mechanism relates back to a theory about cancer proposed almost 100 years ago by the German biochemist Otto Warburg. The old is new again.
The vitamin C – cancer therapy link is now under active investigation by some top-level medical scientists. Watch this space for further developments (or perhaps further disappointments).
Myths can be true.
Go to Latest Posts
Sources
- Siegel, R. L., K. D. Miller, and A. Jemal. 2019. Cancer statistics, 2019. CA Cancer J. Clin. 69:7-34. Available at: https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21551
- Hemila, H., E. Chalker, and B. Douglas. 2007. Vitamin C for preventing and treating the common cold. Cochrane Database of Systematic Reviews.
- Lipton, M. 1973. Task Force Report on Megavitamin and Orthomolecular Therapy in Psychiatry. American Psychiatric Association, Washington, DC.
- Creagan, E. T., C. G. Moertel, J. R. O’Fallon, A. J. Schutt, M. J. O’Connell, J. Rubin, and S. Frytak. 1979. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N. Engl. J. Med. 301:687-690.
- Moertel, C. G., T. R. Fleming, E. T. Creagan, J. Rubin, M. J. O’Connell, and M. M. Ames. 1985. High-dose Vitamin C Versus Placebo in the Treatment of Patients With Advanced Cancer Who Have Had No Prior Chemotherapy. A Randomized Double-blind Comparison. N. Engl. J. Med. 312:137-141.
- Pike, M. C., B. E. Henderson, J. T. Casagrande, I. Rosario, and G. E. Gray. 1981. Oral contraceptive use and early abortion as risk factors for breast cancer in young women. Brit. J. Cancer 43:72-76.
- Lindefors-Harris, B. M., G. Eklund, H. O. Adami, and O. Meirik. 1991. Response bias in a case-control study: analysis utilizing comparative data concerning legal abortions from two independent Swedish studies. Amer. J. Epidemiol. 134:1003-1008.
- Wu, A. H., R. G. Ziegler, M. C. Pike, A. M. Nomura, D. W. West, L. N. Kolonel, P. L. Horn-Ross, et al.1996. Menstrual and reproductive factors and risk of breast cancer in Asian-Americans. Br J Cancer 73:680-686.
- Michels, K. B., C. C. Hsieh, D. Trichopoulos, and W. C. Willett. 1995. Abortion and breast cancer risk in seven countries. Cancer Causes & Control 6:75-82.
- Rosenberg, L., J. R. Palmer, D. W. Kaufman, B. L. Strom, D. Schottenfeld, and S. Shapiro. 1988. Breast cancer in relation to the occurrence and time of induced and spontaneous abortion. Amer. J. Epidemiol.127:981-989.
- Paoletti, X., and F. Clavel-Chapelon. 2003. Induced and spontaneous abortion and breast cancer risk: results from the E3N cohort study. Int J Cancer 106:270-276.




